Palliative Care
Palliative Care
Abhirami Archana Linesh and Dr Lopamudra Das Roy
Published 2020
@BreastCancerHub, All Rights Reserved
Around the globe, people with terminal illnesses, from heart disease to cancer, live with the constant fear of their prognosis or sudden visits to a hospital. This fear provides undesirable stress and pain to patients and their caregivers. So, to give patients the best care possible, both mentally and physically, hospitals around the world have adopted practices in palliative care. In this article, the definition of both palliative care and hospice care is stated in addition to a look into caregiver support and other support groups available around the globe.
What is Palliative Care?
Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with a life-threatening illness.¹ Palliative care is the mental and physical care given to patients as they are fighting a life-threatening disease. That could be anything from psychotherapy and support groups, to pain killers or sedatives. Many hospitals have specific groups of doctors for patients who need attention from all aspects of their health, they are referred to as a palliative care consultation team. To put it in other words:
A palliative care consultation team is a multidisciplinary team that works with the patient, family, and the patient's other doctors to provide medical, social, emotional, and practical support. The team is made of palliative care specialist doctors and nurses, and includes others such as social workers, nutritionists, and chaplains.²
Short history and Stigma
Originally, palliative care did not exist, and hospice care was only practiced in some religious institutions. In 1948, Dame Cicely Saunders, a British physician, founded the first formal hospice in 1948 to care for patients with terminal illnesses.³ Soon the term Palliative care was coined, coming from the Latin word pallium meaning to cloak. From there it has grown into an expansive wing of medicine that has, from its birth, been known to relieve the pain and suffering of its partakers. Although the benefits of palliative care are innumerous, it only recently grew in popularity during the early 2000s.³ As an emerging wing of medicine to enter the spotlight, physicians in various disciplines are still exploring the possibilities of this branch of medicine. Unfortunately, palliative care has been vastly ignored or even shunned in many developing countries; in fact, 75% of countries are not even predicted to have the preliminary integration of palliative care into their health care system.⁴ This is often due to social stigma, physical or financial inability, and the lack of awareness of its benefit. In most of these countries, patients are not aware of palliative care, physicians do not have the option to send patients to one, or patients can not afford the extra expense.
Of course, in addition to the stigma, there is also the difference in opinion between physicians around the globe.
Dr. Sheenu Sheela, a specialist in internal medicine at Atrium Health, North Carolina, United States, says that palliative care provides a holistic approach, to the management of a patient’s symptoms. It can not only manage the physical aspects of symptoms but also the psychological and emotional manifestations. Also, it can be started as soon as the patient is diagnosed with an illness(eg.early incorporation of palliative care at the time of diagnosis of metastatic lung cancer has been shown to prolong survival in that specific patient population). Within her practice, Dr.Sheela has observed early incorporation of supportive oncology(a term which she prefers over palliative care) significantly helping with symptom management in her patients with breast cancer and many other patients undergoing chemotherapy.
On the other hand, a radiation oncologist working in Travancore Medicity, Kerala, India, Dr. Suresh Dutt, says that palliative care in his hospital helps patients with pain management through the prescription of painkillers, like morphine; also that palliative care is usually recommended once a patient has advanced, incurable cancer. These differing opinions are holding back the growth and acceptance of palliative care in various populations.
What About in Developed countries?
Although 14% of countries (mostly European) have advanced levels of palliative care integration into their health system, the stigma reaches well into the patients there as well.⁴ Even in the United States, doctors refrain from saying palliative care for fear of their patient’s concern that it means 'giving up hope'. Instead, they have to use terms like supportive oncology that will make patients less worried over the care they receive. Fortunately, as times keep changing, so do the perspectives of patient populations around the globe; in other words, more and more patients are utilizing the services provided by palliative care for symptom control, nutritional, emotional, and spiritual well being.
An international look at health coverage and the presence of Palliative care.⁴
In a developed country like the United States, an estimated 72% of hospitals with 50 or more beds have palliative care teams and practices.⁵ Unfortunately, the financial costs and conditions related to palliative care also holds the field back from growing. Many hospitals look at financial capabilities, as well as the insurance of the patients when deciding if they can receive palliative care. This is a barrier for many, especially when an estimated 37% of patients with a serious illness (not just cancer) report that they have used up all or most of their savings dealing with their health and medical condition, even though 91% reported having health insurance.⁵ As such, the financial strain that may result from basic treatment may make it extremely hard for patients to receive the palliative care they need. Additionally, in rural places of developed countries, palliative care at the first stages of a disease is simply not feasible because of the financial strain it would put on those low-income patients with only baseline insurance. This is a common trend across the globe: countries in the lower tiers of health coverage usually only have an emerging or recently expanding system of palliative care.
Palliative care for cancer
In general, cancer patients have a higher risk of being clinically depressed; 15-20% of cancer patients were diagnosed as being clinically depressed, according to NCI’s PDQ cancer information summary.⁶ The percent varies with each type of cancer.
Cancer patients specifically may have different causes for their diagnosis of depression. Pain, metabolic or endocrine abnormalities, as well as medication could play a part in a cancer patient's mental health. These varied causes may leave a caretaker of a cancer patient drained; studies conducted show that more than one-third of its surveyed patients with family caregivers noted strains, like emotional, financial, or physical strains, on the caregiver.⁵ The causes may also leave the cancer patient with an unhealthy psychological condition.
These varied reasons increase the importance of Palliative care for cancer patients.
Personal Preference
Not only that, but many patients are also incapable of reporting their preferences in severe conditions. Around 50% of patients reported not being asked their personal preference in case of a critical situation.⁵ So, if a patient wished for a stay at a nursing facility or home in their last minutes, but they were too weak to speak their wishes would go unheard. Putting the patients in a condition that they would not want for themselves.
Thus, palliative care for cancer patients is almost a necessity. Understanding that palliative care can help a cancer patient lead a more healthy life and psychological state through their journey, makes it important for us to speak and raise awareness for it.
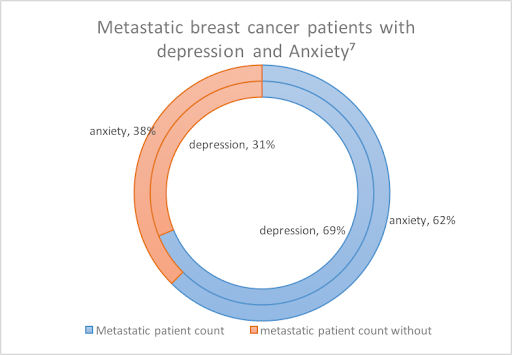
Breast Cancer
Looking specifically at breast cancer, an estimated 30.8% of patients in stage I breast cancer, 30.2% in stage II, and 38.8% percent of patients in stage IV have clinical depression.⁷ For metastatic patients, the figures considerably increase to 68.8% in all areas. Depression, unfortunately, is only one of the numerous mental conditions breast cancer patients can have. The severity of the situation increases when considering that breast cancer is the most common cancer in women, with 1 in 20 women diagnosed with the illness. With such a high population of patients across the globe, we must take further steps in palliative and hospice care to support these people.
What is hospice care?
Hospice care is a part of palliative care that can begin in the last six months of a patient's life. It is important to understand that all hospice treatment is a form of palliative care, but not all palliative care can be considered as hospice care.
To put it bluntly, hospice means that doctors will not treat you for your illness, but rather caregivers will help you get through the symptoms of the illness to produce the ideal last months for a patient. In other words, your pain and other symptoms or side effects will be treated, but not the disease itself. However, it does not have to be a permanent one time only decision. One can even choose whether they wish to enter or leave hospice care. Someone who decided to enroll in it can always choose to leave the program and actually continue with treatment.
Why is it useful?
In the last months of life, it is almost everyone’s wish to be in a caring environment, some may wish that to be at home, others may wish that it will be fighting for their last breath at a hospital, and even some others may prefer a nursing home. When enrolling in hospice, patients can choose where and how they want to be taken care of. This leniency in options and care helps patients take the reins of their end of life treatment, giving them solace and even some peace to the patient's family.
Difference between palliative and hospice care⁴
Caregiver Support
On a patient's cancer journey, one very important person and factor to their recovery is the caregiver(or family). Doctor Dutt, as a specialist in India, comments that it is very difficult to discuss the diagnosis or Prognosis about Cancer directly to the patient due to social factors. So [the doctors] do it with the patient's closest relative. In this example, the family is the main source of comfort for the patient, and the family is the person who speaks on the patient's behalf. This system is common, not only in India but around the world. The role that is placed on the caregiver or family is immense in these cases.
As a result, a patient’s life and recovery can affect their caregivers heavily as well. In a study conducted in England monitoring the behavior of female breast cancer patients’ children, depression was the strongest predictor of emotional and behavioral problems in their children.⁶ This is just a small part of the web, a caregiver may place a patient’s health before their own, neglecting their needs for the patient. This may lead to insomnia or anemia, both extremely harmful for the caregiver.
Caregiver support systems are essential to the health of the patient and their family. Terminal illnesses like cancer can be an emotional and financial drain for patients and their families. Supportive oncology has branches specifically aimed at the health of the caregivers. Dr. Sheela says that the effect of caregiver support (whether that is counseling, psychotherapy, or just a person to talk to) is quite immense, in that it helps the health of the caregiver and saves the patient from thoughts of burdening their caregivers.
Why is support groups important?
Support groups are a cornerstone in the building that is palliative care. As said before, palliative care covers all aspects of health; this includes the social part as well. Support groups give patients and even caregivers places to feel included. As people face breast cancer, their relationships may get strained, they may notice withdrawal of emotion from the people they thought would support them fully.⁸ If this happens, patients must have a group of people that they can trust to support them through their journey.
Of course, many kinds of support groups exist for different reasons; some for the financial aid it can provide for patients, others for the emotional aid, and still some others for the caregivers, family, and doctors who are a part of anyone’s fight against cancer.
Cancer Advocates/Cancer Survivors play a large part in support groups. Advocates are people who have or are fighting or have fought cancer before. Their presence in a support group can motivate an entire group to fight, especially once people see that the end goal is possible.
Unfortunately, support groups are less common in developing countries, just like palliative care. Take India for example, only a handful of cities in a country of 1.353 billion have support groups readily available for patients suffering from any type of disease. They are also extremely hard to find. Dr. Dutt says that support groups are usually only recommended to patients in need of financial aid or for those who are sent home with advanced disease. This creates hopelessness in patients who are advised to join such practices. This stigma must be removed to help people receive the emotional care they need during their journey against cancer (or any other illness).
Support Groups: What they are.
To fully understand support groups you have to understand that there are different aspects of support groups that provide for different functions. For example, some support groups can have open membership, meaning that the people within the group may change often or can have the flexibility of coming and going; meanwhile, other support groups may have closed membership, where once registration is over, the people within the group are expected to always be in the support group till the end of a period.¹º
In addition to the type of group it is, the person who leads the support group can also have a large impact on the group, for example, a support group run by cancer survivors would have a different atmosphere and dynamics, than a cancer support group run by a doctor or psychologist.¹º
There are many different reasons and ways you can participate in a support group, and it is always important to have your options open. To find more about how to design and conduct a support group, visit https://www.breastcancer.org/treatment/comp_med/types/group. To join a support group contact Breast cancer Hub at contact@breastcancerhub.org
Conclusion
As the developing world slowly catches up to the developed nations, new doors into medicine, finance, and transportation are sure to open up for the general population. To achieve this, we must change the idea of disease and care for so many people. We must reach out and educate people who live in remote villages to sprawling cities. We must find new ways to open palliative care to people who may not be able to afford it. We must do that, for a new world of medicine and care.
Works Cited
“WHO Definition of Palliative Care.” World Health Organization, World Health Organization, 28 Jan. 2012, www.who.int/cancer/palliative/definition/en/ .
“What Are Palliative Care and Hospice Care?” National Institute on Aging, U.S. Department of Health and Human Services, 2017, www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care.
Clark, David, et al. “Mapping Levels of Palliative Care Development in 198 Countries: The Situation in 2017.” Journal of Pain and Symptom Management, vol. 59, no. 4, 2020, doi:10.1016/j.jpainsymman.2019.11.009.
America’s Care of Serious Illness: A State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals. Center to Advance Palliative Care and the National Palliative Care Research Center. September 2019
PDQ® Supportive and Palliative Care Editorial Board. PDQ Depression. Bethesda, MD: National Cancer Institute. Updated <04/19/2019>. Available at: https://www.cancer.gov/about-cancer/coping/feelings/depression-hp-pdq. Accessed <07/20/2020>. [PMID: 26389407]
Tsaras, Konstantinos et al. “Assessment of Depression and Anxiety in Breast Cancer Patients: Prevalence and Associated Factors.” Asian Pacific journal of cancer prevention : APJCP vol. 19,6 1661-1669. 25 Jun. 2018, doi:10.22034/APJCP.2018.19.6.1661
“Getting Social Support for Breast Cancer.” Susan G. Komen®, 22 Feb. 2019, ww5.komen.org/BreastCancer/WhatisSocialSupport.html.
Support Groups, Breastcancer.org, 5 May 2020, www.breastcancer.org/treatment/comp_med/types/group.