Dense Breast and Mammogram
Breast Density and the Limitations of Mammograms
Shrika Renganathan & Dr. Lopamudra das Roy
Published 2020
@BreastCancerHub, All Rights Reserved
Dense Breast Tissue
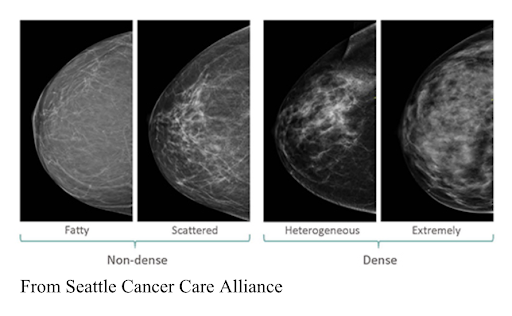
There are four main types of breast tissue: entirely fatty, scattered dense tissue, many areas of dense tissue, and extremely dense tissue. Breast density is often inherited, but a multitude of factors can influence it. For example, fatty breast tissue is common in those who are older and/or have a higher BMI (body mass index) [1]. Dense breast tissue, or tissue that consists of mainly fibroglandular tissue, is found predominantly in those who are younger, have less body fat, and/or take combination hormone therapy for menopause (tamoxifen). Individuals who have dense breasts fall into two categories: heterogeneously dense or extremely dense [2]. Nearly half of all women aged 40 or older who go through mammogram screenings have dense breast tissue. Although this may be true, not all dense-breasted women are above 40 years of age nor are all women above the age of 40 dense-breasted.[3]. There is no way to self-check for breast density. Breast density can only be identified after a mammogram [4] has been conducted so if you have dense breasts, your doctor should include it in your report after the screening [5]. As of now, all 50 states in the US are required to include a patient’s breast density in their reports after mammograms.
Levels of density are described using the American College of Radiology's Breast Imaging Reporting and Data System, which is sometimes shortened to BI-RADS. The levels of density are often included in a mammogram report using letters. The levels of density are:
A: Almost entirely fatty means that the breasts are almost entirely made up of fatty tissue. There is very little dense breast tissue.
B: Scattered areas of fibroglandular density means the breasts are mostly made up of fatty tissue. But there are some scattered areas of dense breast tissue.
C: Heterogeneously dense means that most of the breast tissue is dense breast tissue. But there are some areas of fatty tissue.
D: Extremely dense means that nearly all of the breast tissue is dense breast tissue. There is very little fatty tissue.
Mammograms/Screening
The basic screening for determining whether or not one has breast cancer is a mammogram. A mammogram is, quite simply, a breast x-ray. Just as one would read an x-ray of a bone, a radiologist examines the mammogram for any abnormalities that might be indicative of breast cancer [6]. Most of the time, abnormalities in the breast are non-cancerous growths or cysts. Benign, or non-cancerous tumors may also be present in the breast and will need to be monitored to assure that they will not become cancerous over time. Mammograms are more accurate in those with fatty breast tissue rather than those with dense breast tissue due to the masking of tumors by fibroglandular tissue in individuals with dense breasts [7].
Risk Factors
Women with dense breasts are at a higher risk for breast cancer due to the nature of the tissue itself as well as the limitations of mammogram scans. Tumors and other abnormal growths appear bright white on mammograms whereas fatty breast tissue appears black or grey-ish. This makes it easier to spot possible cancers in those with mostly fatty breasts rather than those with significant amounts of dense breast tissue. On the other hand, tumors go largely undetected in dense-breasted individuals as fibrous connective tissue and glandular tissue also show up as white in mammograms [8]. About 1 in 5 cancers are overlooked by traditional mammograms [9].
Mammogram Discrepancies
Apart from difficulties in locating possible cancerous growths in dense-breasted patients, mammograms can also produce false-negative and false-positive results. False-negative results indicate no presence of any tumors in the breast when there is a tumor in the breast. False-negative results can delay the diagnosis of breast cancer for extended periods, leaving cancer to progress and metastasize throughout the body. False-positive results indicate the presence of a cancerous growth when there are no cancerous growths in the breast. False positives occur around 6-8% of the time and can create unnecessary psychological stress and may require numerous other tests to prove that the said abnormality is cancer [10]. These results are more common in those who have dense breasts, are younger, have had previous biopsies, have a family history of breast cancer, and/or are taking estrogen supplements. Usually, false positives occur during one’s first mammogram and the chances of a false positive drop by almost 50% if the patient has a previous mammogram for comparison [11].
Alternative Testing Options
Multiple additional tests can be conducted for those who have been found to have dense breasts. These include 3D mammograms (or breast tomosynthesis) and breast ultrasounds. Many women opt for an additional 3D mammogram, especially if they have dense breasts. These mammograms involve getting images from various angles to formulate a 3D image of the breast. 3D mammograms increased the rate of breast cancer diagnosis by around 40%. Although this method is a better detector of breast cancer and many mammography centers are combining the traditional mammogram with 3D mammograms, these tests may not be covered by insurance in some places [12]. Both the traditional mammograms and 3D mammograms involve minuscule amounts of radiation that usually do not pose much of a risk, but may accumulate over time. Most of the time, women are susceptible to breast cancer above the age of 40, but that does not completely minimize the risk for those who are younger.
Dense-breasted women can also consult their physician and request a breast ultrasound. This form of screening does not require any radiation and uses sound waves to analyze the breast tissue. Although these are used mainly to closely examine areas of concern on mammograms, they can also be used to scan an entire breast for abnormalities. Ultrasound imaging of breasts has been proven to increase cancer detection by around 40% according to twenty-nine studies conducted since 2000 [13]. These tests are extra additions as well, so ultrasounds may not be covered by insurance. Ultrasounds are sometimes covered by insurance companies only after multiple mammograms are conducted.
Awareness
Although there are widespread awareness and availability of breast cancer screenings across the United States, women are refraining from getting screened due to the taboos that surround breasts and breast cancer, and are ending up with diagnoses of metastatic breast cancer that could have been caught early and treated. In other parts of the world, women are much less likely to get mammograms due to the stigma surrounding such topics. As a result, many do not get a clear idea of their breast density. These occurrences are greater in undeveloped countries where limited access to scans is also a major concern. Even if there are opportunities to get 3D mammograms and ultrasounds, many are not aware of such opportunities. There has been little to no awareness in this area and this has been emphasized by the lack of comparative studies between developed and undeveloped countries. To maintain a healthier population, we must normalize topics concerning breast health and diagnosis.
Breast Cancer Hub strives to discuss the effective screening processes for those with dense breasts, analyze and educate about the environmental factors/workplace hazards that contribute to breast cancer, provide support to those who have been impacted by cancer, and break the taboo around breast health.
Works Cited
1. Carney, P. A., Miglioretti, D. L., Yankaskas, B. C., Kerlikowske, K., Rosenberg, R., Rutter, C. M., . . . Ballard-Barbash, R. (2003). Individual and Combined Effects of Age, Breast Density, and Hormone Replacement Therapy Use on the Accuracy of Screening Mammography. Annals of Internal Medicine, 138(3), 168. doi:10.7326/0003-4819-138-3-200302040-00008
2. Dense breast tissue may increase the risk of breast cancer. (2020, February 18). Retrieved August 12, 2020, from https://www.mayoclinic.org/tests-procedures/mammogram/in-depth/dense-breast-tissue/art-20123968
3. Cancer.gov. (2020). Dense Breasts: Answers to Commonly Asked Questions. Retrieved August 12, 2020, from https://www.cancer.gov/types/breast/breast-changes/dense-breasts
4. AreYouDense. (2020). New JACR Study Shows Dense Breast Reporting Laws Significantly Increase Breast Density Awareness, Conversations Between Women and Physicians on Screening. Retrieved August 12, 2020, from https://www.areyoudense.org/news-events/new-jacr-study-shows-dense-breast-reporting-laws-significantly-increase-breast-density-awareness-conversations-between-women-and/?pageNumber=1
5. AreYouDense. (2018). Are You Dense? Exposing the Best-Kept Secret.Retrieved https://www.areyoudense.org/files/1615/1483/5617/2018.two_page_brochure_ENGISH.pdf
6. CDC. (2018, September 11). What Is a Mammogram? Retrieved August 12, 2020, from https://www.cdc.gov/cancer/breast/basic_info/mammograms.htm
7. Hopkins. (2020). Mammogram Procedure. Retrieved August 12, 2020, from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/mammogram-procedure
8. Cancer.org. (2019, June 26). Dense Breasts: Breast Cancer Risk Factors. Retrieved August 12, 2020, from https://www.breastcancer.org/risk/factors/dense_breasts
9. UCHealth, B. (2019, February 05). How Accurate Are Mammograms? Retrieved August 12, 2020, from https://www.uchealth.org/today/how-accurate-are-mammograms/
10. Cancer.org.(2020). Limitations of Mammograms: How Often are Mammograms Wrong/ Retrieved August 12, 2020, from https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/limitations-of-mammograms.html
11. 3D Mammography More Likely to Find Small Invasive Breast Cancers, Especially in Women Younger Than 50. (2019, June 26). Retrieved August 12, 2020, https://www.breastcancer.org/research-news/3d-mammos-more-likely-to-find-small-invasive-bc
12. AreYouDense. (n.d.). Ultrasound increases 40% detection over mammography for dense breasts. Retrieved August 12, 2020, from https://www.areyoudense.org/resources/research-dense-breast-tissue/ultrasound-increases-40-detection-over-mammography-dense-breasts/?pageNumber=1
13. Dense breast tissue may increase the risk of breast cancer. (2020, February 18). Retrieved August 12, 2020, from https://www.mayoclinic.org/tests-procedures/mammogram/in-depth/dense-breast-tissue/art-20123968