Benign Breast Tumor
Benign Breast Conditions
Sanjana Surapaneni, Dr. Lopamudra Das Roy
Published 2020
@BreastCancerHub, All Rights Reserved
Comprehending Cancer¹
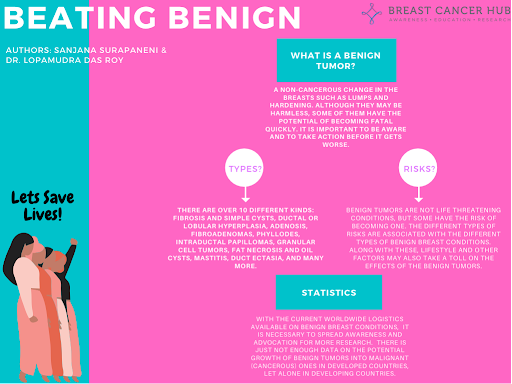
Cancer is essentially the overgrowth of the body’s cells. Normally, cells go through a cycle in which they grow and reproduce as needed, and some even die after reproducing several times. Cancer occurs when something goes wrong in the life cycle of these cells and the cells begin to rapidly reproduce and not die. The accumulation of these overgrowing cells is referred to as a tumor. Tumors are classified into two groups: Benign and Malignant.
Benign Tumors¹
Benign breast tumors are non-cancerous and are extremely common in women. While breast cancer is life-threatening, benign tumors are not, in fact, many changes in the breast are considered to be benign. Although they are considered non life-threatening, some benign tumors have the potential of spreading and transforming into breast cancer. Some changes may not be found during a mammogram (x-ray of the breasts) and may not cause any symptoms, whereas some changes can cause symptoms very similar to the ones caused by breast cancer. This makes it difficult to differentiate between benign tumors, which are non-cancerous, and breast cancer, which is life-threatening.
Types of Non-Cancerous Breast Conditions²
There are over 10 different kinds of non-cancerous breast conditions: Fibrosis and Simple Cysts, Ductal or Lobular Hyperplasia, Adenosis, Fibroadenomas, Phyllodes, Intraductal Papillomas, Granular Cell Tumors, Fat Necrosis and Oil Cysts, Mastitis, Duct Ectasia, and many others.
Fibrosis and Simple Cysts (low risk/some may cause a slightly larger risk)
Many breast lumps can be classified as fibrosis and/or cysts, which is very common amongst women. Fibrosis is large amounts of fibrous tissue (which makes up scars) that forms lumps in the breast. Cysts are fluid sacs within the breast. They typically form in women in their 40s, but can occur at any age. Hormonal changes in the body may cause them to enlarge and even become painful, especially before the menstrual cycle.
Mostly, fibrosis/cysts are diagnosed based on symptoms like breast lumps, swelling, and tenderness/pain. Occasionally, one of the lumps may be firmer or look different from the other, causing concerns about breast cancer. When this happens, doctors perform an ultrasound to determine whether it is a solid lump, or if its fluid, which is classified as a cyst. If all of it is solid, or part of it, then a biopsy (removal of part or all of the tumor for testing) may be done to ensure that it is not cancerous.
Fibrosis and simple cysts do not necessarily increase your chances of getting breast cancer later on, but complex cysts, which are part fluid and part solid, may contain cancer, or slightly increase chances of getting breast cancer, depending on the biopsy results.
Hyperplasia of the Breast: Ductal or Lobular (risk depending on type)
Hyperplasia is the increased growth of cells that line the ducts (ductal hyperplasia) or the lobules, also known as milk glands, (lobular hyperplasia) inside of the breast. Hyperplasia is divided into two categories: usual, where the cells look very close to normal, and atypical, where the cells grow in an abnormal pattern.
Hyperplasia does not typically cause a lump that can be felt, but it can cause abnormalities seen in mammograms, which is diagnosed by a biopsy.
Depending on the type of hyperplasia, the risk for breast cancer can vary. For mild hyperplasia of the usual type, it does not increase the risk for breast cancer, but for moderate hyperplasia of the usual type, the chances double compared to a person with no breast abnormalities. With atypical hyperplasia, the risk becomes 4 to 5 times higher.
Adenosis (low risk)
Adenosis is a condition where the lobules (milk-producing glands) become enlarged, and there are more glands than normal. It is usually found in those who have fibrosis or cysts in their breasts.
If the enlarged lobules are super close to each other, it may be hard to differentiate the lump from adenosis of breast cancer. Mineral deposits, common to both adenosis and breast cancer, may also make it difficult to differentiate using a mammogram. This is why biopsies are usually needed. They are usually not treated unless it leads to severe symptoms.
Fibroadenomas of the Breast (risk depending on type/typically low risk)
Fibroadenomas are made up of both glandular and stromal tissue and are very common benign tumors. They are most common from the ages of 20-30, but can be found in any age. After menopause, they typically shrink.
Some are too small to feel, while some are much bigger. They can move around under the skin and have a firm, rubbery feel to them. They are typically found using a mammogram, but a biopsy is needed to ensure it is a fibroadenoma and not a tumor.
Complex fibroadenomas, which are typically bigger, pose a slightly bigger threat to developing breast cancer later on compared to the risks simple fibroadenomas present.
Phyllodes Tumors of the Breast (low risk)
Phyllodes tumors are rare and are conceived in the connective tissue of the breast. They are typically found in individuals in their 40s, but once again, they can occur at any age. Although most are considered benign, 1 out of every 4 of them are considered malignant (invasive cancer).
They are usually painless lumps, but they can sometimes hurt. Ultrasounds or mammograms usually spot them first, but this causes them to be confused with fibroadenomas. This is why the diagnosis is often made with a biopsy. Sometimes, the whole tumor needs to be removed in order to ensure it is a benign tumor, not a malignant one.
A phyllodes tumor does not affect the risk of developing breast cancer, but patients with the condition get more imaging tests to ensure the tumor did not return after the surgery.
Intraductal Papillomas (single-low risk/multiple-increased risk)
Intraductal papillomas are tumors that grow in the milk ducts. They consist of gland and fibrous tissue along with blood vessels. The tumors may feel like a small lump close to the nipple and may cause nipple discharge.
When diagnosing papillomas, ductograms, which are x-rays of the breast ducts, are used to find the papillomas while an ultrasound or mammogram may be done to inquire about the size and location of it. A biopsy is also possible if the papilloma is large enough.
A single papilloma, referred to as solitary papilloma, does not lead to breast cancer risk unless it is paired with other breast deformities. Having multiple papillomas does, however, increase the risk for breast cancer.
Granular Cell Tumors of the Breast (very low risk)
Granular cell tumors appear in the early stages of nerve cells, and are very rarely found in the breast. If it is in the breast, it is felt as a firm lump that is moveable or attached to the skin. Most of them occur in the upper part of the breast.
Mammograms and ultrasounds are used to get more information about the size, shape, and location of the tumors. They are confused with cancer because they are in a fixed position and can appear as cancer on the mammograms, but to avoid a false diagnosis, a biopsy is once again used to ensure the identity of the tumor.
The tumors are almost never linked to a higher chance of getting breast cancer.
Fat Necrosis and Oil Cysts in the Breast (very low risk)
Fat necrosis is a benign condition that occurs when there is damage to the fatty breast tissue, generally caused by injury, surgery, or radiation treatment. When damaged, the breast is repaired with firm scar tissue. While most cells will respond like this, some may die and release their own contents instead of forming scar tissue. Forming sacs filled with greasy fluids (oil cyst).
The skin around the necrosis and oil cysts is normally thicker, and sometimes even bruised. This makes it difficult to differentiate from cancers on examinations and even mammograms. Most times, doctors will use biopsies instead.
These types of benign breast tumors do not typically increase the risk of getting breast cancer.
Mastitis (very low risk)
Mastitis is the inflammation in the breast, usually caused by an infection. It mostly affects women who are breastfeeding, but can affect other women as well. A clogged duct, not having a breast fully drained of milk, and bread in the nipple are all issues that cause the body’s white blood cells to release substances to fight it. This leads to swelling and inflammation.
It is usually diagnosed through breast examination and the symptoms listed by the patient, and generally, it only affects one breast.
Having mastitis does not increase the chances of getting breast cancer.
Duct Ectasia (very low risk)
Duct ectasia occurs when a milk duct widens and the wall of the duct thickens. This leads to blockage and fluid build-up. Most common among women that are getting close to menopause.
Many times, there are no symptoms, and it is only found when a biopsy is performed for another reason. An ultrasound or mammogram may be performed if the nipple begins to discharge, and if it appears to be pulled inward with redness because it is often confused with cancer. Ultimately, a biopsy is used if there is a lump to ensure it is not cancer.
This benign condition also doesn’t increase your chances of breast cancer.
Radial Scars (slight risk)
Radial scars are found when a biopsy is performed for another reason, and they typically distort the breast tissue. They are important because if they are large, they may be classified as cancer on a mammogram or biopsy, and they may be linked to an increase in developing breast cancer in the patient.
Other benign conditions include Lipoma (a fatty tumor that can occur anywhere in the body), Hamartoma (a smooth lump formed by overgrowth of breast cells), Hemangioma (a tumor made of blood vessels), Adenomyoepithelioma (a tumor formed by cells in the milk duct walls), and Neurofibroma (an overgrowth of nerve cells). These conditions do not lead to any increases in the risk of getting breast cancer, but they may be removed through a biopsy to ensure they do not contain cancerous cells.
Risks
Benign tumors tend to grow in a fixed location in the body. They can’t spread or begin to invade other parts. Despite this, many benign tumors that form in or around any vital organs such as the heart or brain tend to be dangerous. This leads to the surgical removal of the tumor which is also used if the tumor needs to be checked for any dangerous cancer cells or to clarify it is benign and not malignant.³
However, if left untreated, some benign tumors have the potential of becoming a life threatening condition. Some benign tumors, if not detected early or if they are ignored, can grow out of control. Eventually, they will grow to the point where some of the cancerous cells from the tumor will enter the body’s bloodstream. Through the blood, these cancerous cells will spread to other parts of the body and even major organs. This causes the cancer to spread and transforms a benign tumor, where the tumor remains in one place, to a malignant tumor, which has spread rapidly to the body. Malignant cancers are incredibly difficult to treat, so it is extremely important to take precautions and always keep an eye on benign tumors so that they do not spread, or in some cases, lead to increases in the chance of getting breast cancer later on.³
Sometimes mammograms tend to miss breast cancer. Although benign tumors are not cancerous, and many of them are at low risk of becoming invasive cancer, it is extremely crucial to keep an eye out for any changes. This is why it is probably best to get a breast ultrasound done to ensure the benign tumor is not cancerous. If there is further suspicion, a biopsy is another great way to provide surety on what type of change the breast has undergone. But relying on the results, and not following up with check ups is a very dangerous mistake. Always make sure to keep getting checked if you have a benign tumor so that it doesn’t grow into something uncontrollable.⁴
Many experts often place benign tumors into three categories based on how the tumor may increase the chances of developing breast cancer in the individual: no increase in risk, slight increase in risk, and moderate increase in risk. The “no increase” and “slight increase” don’t require much treatment other than the regular screenings, but the “moderate increase” may require more frequent screenings.⁵
Sometimes, benign tumors may feel lumpy and can cause discomfort/pain. It is important to get it checked, and possibly surgically removed, to ensure that it does not become malignant. Even if a benign tumor has been surgically removed, certain kinds such as fibroadenoma, come back.⁶
Risk Reduction⁵-
Lifestyle changes can help reduce the risk of breast cancer. For example, keeping a clean diet, exercising regularly, no smoking, and drinking low amounts of alcohol are all lifestyle factors that can be changed to aid in prevention.
If the patient is at a moderately increased risk, then it may be suggested that they take medicines such as Nolvadex (tamoxifen) or Fareston (toremifene). These medicines are effective in lowering hormonal levels in the body, reducing the risk of hormone-receptor-positive breast cancer.
Benign Tumor Statistics
Across the US and in developing countries, there may be statistics on the amount of women diagnosed with invasive breast cancer, there is rarely any data on the rates of benign breast cancer amongst women. Although it is extremely important to raise awareness of metastatic cancer, it is equally as important to research and statistically gather data about the rates of women diagnosed with benign tumors and subsequently, how many of these cases grow into malignant/cancerous tumors. Without this data, many women become negligent with their benign breast changes, and this negligence transforms into something they cannot control. This type of research needs to be promoted not only to help promote awareness of the possible dangers of benign tumors, but also to encourage women for regular mammograms, breast screenings, etc. The more we promote prevention, lesser women will become victims of metastatic breast cancer.
As seen in the graph on the left, atypical hyperplasia, a high-risk benign breast tumor, has the potential of growing over 10% within the range of five years. This exponential increase is a drastic change that many women are not aware of. Although other benign tumors may not grow as drastically, if ignored, it can begin to grow similar to what is depicted in the graph. With this type of potential growth in benign tumors, it is incredibly essential, now more than ever, to spread awareness of the risks of benign tumors, and to continually push for more research to be done. Especially in the developing countries. Currently, finding data on the rates of benign tumors turning into malignant tumors is extremely low in the US, a developed country, while developing countries don’t even have statistical data available on invasive breast cancer (a more common research topic).⁷
References
Cancer 101. (n.d.). Retrieved August 06, 2020, from https://www.americancancerfund.org/cancer-101/?gclid=CjwKCAjwsan5BRAOEiwALzomX5UFQ6PY-ZghK2UrZRODqMEbjxR0HnTsOCCdyGD3-kMIH8QtNKwPgRoC4tMQAvD_BwE
Non-cancerous Breast Conditions: Breast Fibroids. (n.d.). Retrieved August 06, 2020, from https://www.cancer.org/cancer/breast-cancer/non-cancerous-breast-conditions.html?fbclid=IwAR2Pax2t6tTiLMoDj_4fp0RUEUfNm5NG7TJeELbpgOmL7Zo_-VeoZQQ5QTc
Benign Tumors. (2020, July 01). Retrieved August 06, 2020, from https://medlineplus.gov/benigntumors.html
Limitations of Mammograms: How Often are Mammograms Wrong? (n.d.). Retrieved August 22, 2020, from https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/limitations-of-mammograms.html
Benign Breast Conditions. (2020, February 05). Retrieved August 06, 2020, from https://www.breastcancer.org/symptoms/benign
Benign Breast Disease Management and Treatment. (n.d.). Retrieved August 06, 2020, from https://my.clevelandclinic.org/health/articles/6270-benign-breast-disease/management-and-treatment
Santen, R. (2018, May 25). Benign Breast Disease in Women. Retrieved August 22, 2020, from https://www.ncbi.nlm.nih.gov/books/NBK278994/